Cryoablation stands out as a highly effective palliative treatment option for individuals grappling with pancreatic cancer, offering a range of benefits that contribute to an improved quality of life. It has the advantage of minimal invasion and can safely bring less pain to patients, ultimately leading to less postoperative pain and a quicker recovery period.
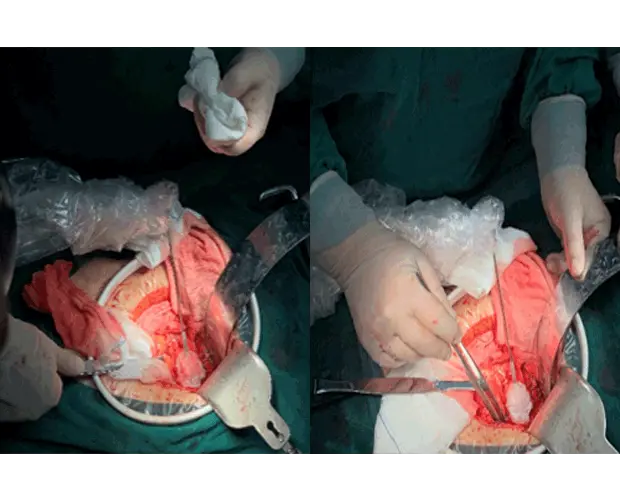
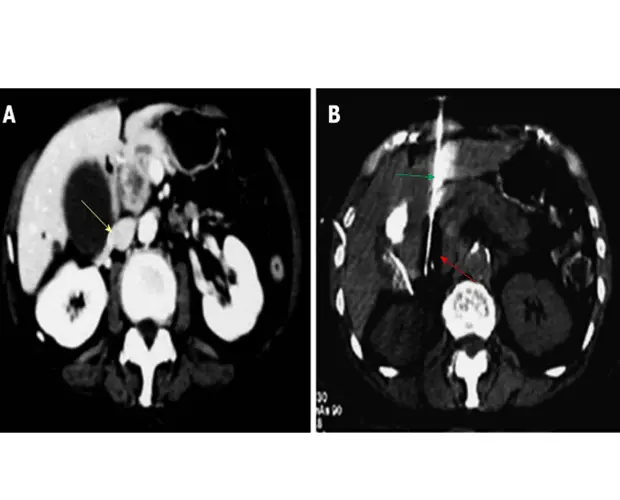
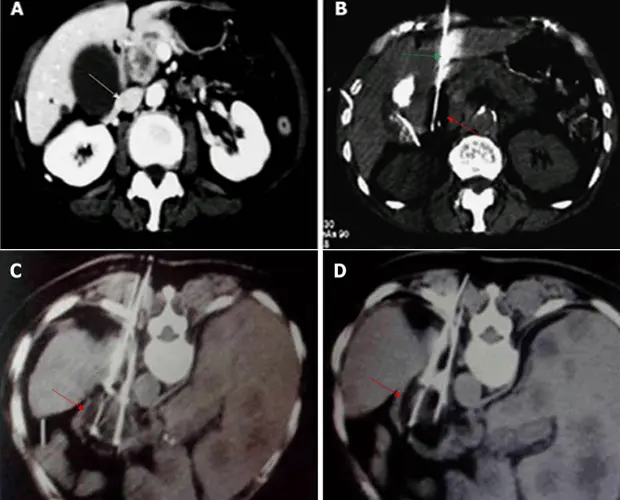
Treatment pathway of cryoablation:
1. Treatment of pancreatic head tumors through the transabdominal approach. This method allows for the controlled application of extreme cold temperatures to freeze and subsequently destroy the cancerous cells, effectively impeding the progression of the disease.
2. Treatment of tumors located in the body or tail of pancreas through dorsal approach. In cases where tumors are located in the body or tail of the pancreas, a dorsal approach is adopted during cryoablation. This targeted technique ensures the thorough treatment of tumors situated in these regions, further expanding the applicability of cryoablation across various pancreatic cancer presentations.
The significance of cryoablation extends beyond its technical approach, encompassing a holistic patient-centric perspective. By minimizing invasion and mitigating pain, cryoablation not only addresses the physiological aspects of pancreatic cancer but also attends to the emotional and psychological well-being of individuals undergoing treatment. This comprehensive approach underscores the importance of integrating innovative and patient-friendly interventions in the ongoing battle against pancreatic cancer, offering a ray of hope for those facing this challenging diagnosis.




 Hygea Medical Technology Co., Ltd.
Hygea Medical Technology Co., Ltd.