GUAN Haitao1, LI Tiantian2, FAN Zeyang1, WANG Jian1, ZOU Yinghua1*
(1. Department of Interventional Radiology and Vascular Surgery, Peking University First Hospital, Beijing 100034, China; 2. Department of Gastroenterology, Feicheng People's Hospital, Taian 271600, China)
[Abstract] Objective To observe the short-term efficacy and safety of CT-guided percutaneous compound cryoablation for liver malignancies. Methods Data of 45 patients with malignant liver tumor who underwent CT-guided percutaneous compound cryoablation (Combo knife) were retrospectively analyzed, including 20 cases of primary hepatocellular carcinoma (HCC) and 25 cases of liver metastases. Totally 50 liver lesions were treated, including curative ablations of 20 lesions (18 cases, 16 cases with 1 and 2 cases with 2 lesions) and palliative ablations of 30 lesions (27 cases, 25 cases with 1, 1 case with 2 and 1 case with 3 lesions). Intraoperative and postoperative adverse reactions were recorded. Enhanced abdominal CT or MR were re-examined1, 3 and 6 months after treatments, and the therapeutic efficacies were evaluated according to the modified-response evaluation criteria in solid tumors (mRECIST). Results All 45 patients successfully completed ablation, 37 underwent single needle ablation and 8 received double needle ablation. Small amount of fluid accumulation or blood around the liver were noticed in 6 cases during and after treatments, mild local skin frostbite during operation occurred in 1 case, mild nausea complained after treatment by 8 cases, all improved spontaneously or after symptomatic treatment. Among lesions after curative ablation, complete remission (CR) was found in all 20 lesions 1 month after treatment, while 19 (19/20, 95.00%) CR and 1 (1/20, 5.00%) progressive disease (PD) were observed 3 and 6 months after treatment. Among lesions after palliative ablation, partial remission (PR) was found in 25 (25/30, 83.33%) lesions and stable disease (SD) was detected in 5 (5/30, 16.67%) lesions 1 month after treatment, while 22 (22/30, 73.33%) of PR, 7 (7/30, 23.33%) of SD and 1 (1/30, 3.33%) of PD were noticed 3 months after treatment, and 17 (17/30, 56.67%) of PR, 7 (7/30, 23.33%) of SD and 6 (6/30, 20.00%) of PD were observed 6 months after treatment. Conclusion The short-term efficacy and safety of CT-guided percutaneous compound cryoablation for liver malignancies were both good.
[Keywords] liver neoplasms; cryoablation; tomography, X-ray computed
[CLC No.] | R735.7; R815 | [Document code] | A | [Article No.] | 1672-8475(2023)04-0198-04 |
DOI: 10. 13929/j. issn. 1672-8475. 2023.04.002
Liver cancer is a clinically common malignant tumor, which ranks the front position in morbidity and mortality among malignant tumors, with poor prognosis [1]. Surgical resection is the main treatment for early liver cancer, and local treatment represented by ablation has equivalent efficacy as surgery for most of early liver cancer [2]; middle and advanced liver cancer has lost the chance of radical surgery, and is often treated by local treatment combined with systemic treatment at present [3]. The cryoablation has accurate local inactivation effect of lesions, and it can achieve radical curative effect for some early tumour. After treatment, the tumor antigen exposure may enhance the body's anti-tumor immune response, thus having a synergistic effect with systemic therapeutic drugs [4-5]. This study was performed to observe the short-term effect and safety of co-ablation system (Combo knife) with liquid nitrogen as refrigerant in the treatment of liver malignancies.
1.1 General data: A retrospective analysis was performed on 45 patients with liver malignancies underwent CT-guided percutaneous compound cryoablation in Peking University First Hospital from July 2019 to June 2021, including 33 males and 12 females, aged 31 - 72 years old, with median age of 60.5 years old; including 20 patients with primary hepatocellular carcinoma (HCC) and 25 patients with hepatic metastasis (for primary lesions, 20 patients with colorectal cancer, 2 patients with gastric cancer, 2 patients with pancreas cancer and 1 patient with adrenal carcinomas); 26 patients were diagnosed by pathology, and 19 patients were diagnosed by a combination of medical history, imaging and laboratory examination. 26 patients had single lesion and 19 patients had multiple lesions. A total of 50 lesions were treated, with a long diameter of 11.5~98.6 mm, a median long diameter of 62.1 mm, a short diameter of 11.0~93.6 mm and a median short diameter of 59.4 mm; 18 patients underwent radical ablation (20 lesions in total, 1 in 16 patients, 2 in 2 patients, maximum diameter ≤ 5 cm, with clear boundary and regular shape, no invasion of great vessels, diaphragm and adjacent important organs), and 27 patients underwent palliative ablation (30 lesions in total, 1 in 25 patients, 2 in 1 patient and 3 in 1 patients, maximum diameter > 5 cm, with unclear boundary, irregular shape and infiltrative growth, complete ablation not expected). Acceptance criteria: ① There was no indication of ablation or the patient was reluctant to undergo ablation; ② There were indications of ablation therapy, and patients can tolerate surgery. The patients with severe cardiopulmonary dysfunction and coagulation dysfunction were excluded. Before operation, patients and their families signed the informed consent.
1.2 Instruments and methods: GE Discovery CT750 HD CT machine was used as interventional guidance device; the ablation device is the co-ablation system (Combo knife) and disposable sterile cryoablation needle (14G, 15 cm or 18 cm in length). The inserting site, path and number of needles were determined according to preoperative imaging data. Asked the patient to lie on the back or in the right anterior oblique position, and give ECG monitoring and oxygen inhalation. After CT scan was performed to determine the puncture point, 2% lidocaine was used to locally anesthetize the skin at the puncture point, the syringe needle was allowed to leave in the body, and scanning was performed again to measure the angle and length of the needle with the needle as a reference. Made a small incision in the skin at the puncture point, adjusted the angle and depth of the needle to allow the needle percutaneously puncture to the lesion, and connected the co-ablation system before starting ablation treatment after CT scan confirmed that the position of the ablation needle is satisfactory. The two-cycle ablation method was adopted. To be specific, rewarming for 5 - 8 min after cryoablation for 15 min, then rewarming again for 5 min after cryoablation for 10 -15 min, with an interval of 5 - 10 min. During this period, the position of ablation needle and the coverage of lesion by the ice ball were observed through CT scan. If necessary, the position of ablation needle was adjusted. Repeat the procedure above. When radical ablation was performed, the ice ball shall be arranged 5 ~ 10 mm beyond the edge of the lesion; when palliative ablation was performed, the ice ball shall be arranged to cover the lesion as fully as possible. After the ablation reached a satisfactory range, heat treatment was performed for the needle passage, then the needle was pulled out, and the whole abdomen CT scan was performed to observe whether there were complications such as bleeding. If necessary, symptomatic treatment shall be performed. After radical ablation, if the lesion remains or develops further during the observation period, cryoablation therapy shall be performed for a second time; after palliative ablation, the lesions were treated with chemotherapy, targeting and immunization according to pathological types.
1.3 Observation indexes and follow-up: The adverse reactions and complications were observed during ablation and within 4 weeks after ablation. Abdominal enhanced CT or MRI examination was performed at 1, 3 and 6 months after operation, and the treatment effect was evaluated according to the modified-response evaluation criteria in solid tumors (mRECIST), that is, complete response (CR), partial response (PR), stable disease (SD) or progressive disease (PD).
2.1 General information: 45 ablation therapies were successfully completed (Figures 1 and 2), with single needle adopted for 37 patients and double needle adopted for 8 patients. 32 patients of whom the lesion could not be accurately located and the boundary of the lesion could not be determined by plain CT scan before operation were treated with lipiodol-based super-selective TACE on the 2nd day before operation to mark lesion, and 13 patients directly underwent CT-guided ablation. 18 patients received radical ablation for 20 times (twice for 2 patients, once for 16 patients), among whom 6 patients maintained systemic treatment after operation, and 12 patients received ablation treatment only; 27 patients received one-time palliative ablation, among whom 21 patients maintained systemic treatment after operation, and 6 patients received no other treatment.
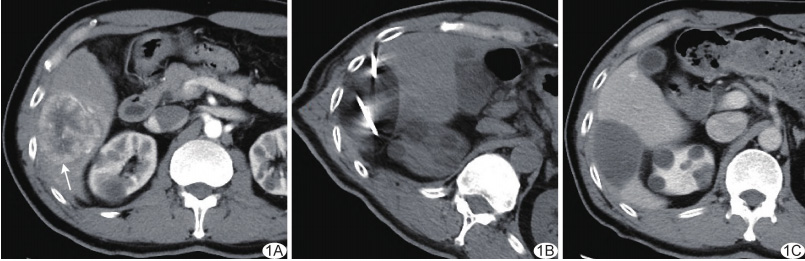
Figure 1 A 64-year-old male patient with primary HCC. A. Preoperative axial CT of abdominal enhanced artery showed a 4.6 cm x 4.9 cm lesion (arrow) in the S6 segment of right lobe of liver, which was obviously enhanced. B. Radical ablation was performed with double needles, and the ice ball area was fully covered according to the axial plain CT scan during the operation; C. Three months after operation, the axial CT scan of abdominal enhanced artery showed that the ablation focus had clear edge and there was no enhancement, with an efficacy evaluated as CR.
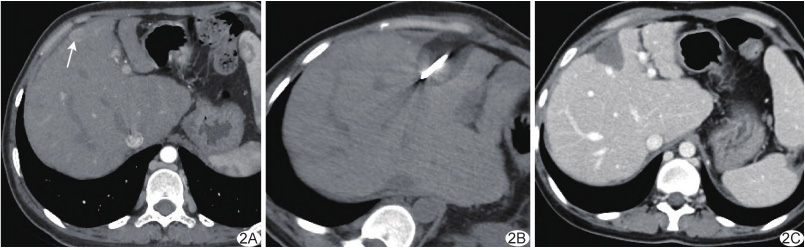
Figure 2 A 38-year-old female patient with primary HCC. A. Preoperative axial CT of abdominal enhanced artery showed a 1.6 cm x 1.2 cm lesion (arrow) under the horizontal capsule of S4 segment of left lobe of liver, which was obviously enhanced. B. Radical ablation was performed with a single needle, and axial plain CT showed that the ice ball completely covered the lesion during the operation; C. One month after operation, the axial CT of abdominal enhanced artery showed that the ablation focus had clear boundary and there was no enhancement, with an efficacy evaluated as CR.
A small amount of hematocele or effusion appeared around the liver in 6 patients during and immediately after operation, and they did not experience any significant discomfort. One patient suffered mild frostbite on local skin during operation. After operation, 8 patients had mild nausea with or without vomiting, and they were relieved automatically or after symptomatic treatment.
2.2 Efficacy: The efficacy of 20 patients reached CR after one month of radical ablation. 19 lesions (19/20, 95.00%) showed CR and 1 lesion showed PD (1/20, 5.00%) in 3 and 6 months after operation. Among 30 palliative ablation lesions, 25 lesions (25/30, 83.33%) showed PR and 5 lesions (5/30, 16.67%) showed SD one month after operation, and 22 lesions (22/30, 73.33%) showed PR, 7 lesions (7/30, 23.33%) showed SD and 6 lesions (6/30, 20.00%) showed PR three months after operation.
As one of the local minimally invasive ablation treatments, cryoablation has been used in many solid malignant tumors [6-9], and its treatment effect on early solid malignant tumors is equivalent to that of hyperthermia ablation technology such as radio frequency and microwave, without the requirement of general anesthesia [10].
In this study, CT-guided percutaneous compound cryoablation radical ablation was performed for malignant tumors in the liver by using co-ablation system (Combo knife). In the two-cycle treatment mode, the elliptical ice ball with a length of about 3 cm x 5 cm can be obtained by using Combo knife with single needle ablation. For the lesions with the largest diameter of less than 3 cm, single needle may meet the treatment needs, but the needle planning was required according to the position and shape of the lesions before the operation to allow the ice ball cover the lesions as fully as possible, and adjust the insertion angle for repeated ablation if necessary, with a relatively long treatment time. Double-needle or three-needle mode can obtain a wider range of ice ball in unit time. No matter radical or palliative treatment, a larger ablation zone can be obtained by multi-needle layout and increasing treatment cycle.
This group of patients had primary and secondary liver malignancies, and patients may have single or multiple lesions. For some patients with multiple lesions, not all lesions had been ablated, but only those with indications of treatment were ablated locally. The evaluation effect is only for the ablated lesions, not for the patient's overall disease. Affected by the effective range of the device and the location of the lesion [11], it is often difficult to achieve radical ablation for large or irregular lesions. At this time, the palliative treatment can be provided with a purpose of reducing tumor, relieving symptoms and activating tumor immune response, which will provide the possibility for subsequent combined chemotherapy, targeted and immune treatment [12].
Currently, when performing radical ablation, it is believed that the ablation zone should be at least 5-10 mm beyond the lesion edge to effectively reduce the local recurrence [13]. The range of ice ball obtained by cryoablation is usually larger than the actual necrosis range. The required safety margin is larger when ice ball is taken as a reference, so the ablation zone should be expanded as much as possible under the premise of ensuring safety [14]. If CT shows that the lesion is not good, TACE can be performed with lipiodol before ablation to better locate or delineate the boundary of the lesion.
This group of patient (20 lesions) underwent radical ablation. The CR rate was 95.00% (19/20) three and six months after operation, and there was a PD lesion near the diaphragmatic apex. Considering that it was related to the insufficient ablation zone, it was suggested that more attention should be paid to the lesions near special parts such as great vessels and diaphragmatic apex on the basis of full familiarity with the performance of the device [15]. 30 lesions were treated with palliative ablation, and the tumor was clearly necrotic one month after operation, but the residual part of the tumor progressed slowly with time, and 6 lesions were evaluated as PD six months after operation, so the combination of systemic treatment is required.
Common complications of cryoablation include postoperative pain, nausea and vomiting, bleeding and infection, and rare complications include frostbite and cold shock. A small amount of hepatic capsule hematocele and effusion can be absorbed by itself without special intervention, and those with severe pain, nausea and vomiting can be treated appropriately. Strengthening the protection of low temperature pipeline during operation can effectively avoid skin frostbite. The incidence of intraoperative and postoperative complications in this group was about 33.33% (15/45), mainly manifested as mild nausea, a small amount of blood around the liver, etc. One patient was subjected to local skin frostbite during operation and recovered after topical medication, and no serious complications were found [16].
To sum up, the short-term efficacy and safety of CT-guided co-ablation system in the treatment of liver malignancies are good. Limitations of this study: ① Retrospective study with small sample size; ② Not compared with other treatment methods; some patients treated in combination with systemic treatment failed to be evaluated by classification; ③ Short follow-up time; follow-up needs to be further strengthened.
[References]
[1] ZHANG C H, CHENG Y, ZHANG S, et al. Changing epidemiology of hepatocellular carcinoma in Asia [J]. Liver Int, 2022, 42(9): 2029-2041.
[2] SHIINA S, SATO K, TATEISHI R, et al. Percutaneous ablation for hepatocellular carcinoma: Comparison of various ablation techniques and surgery [J]. Can J Gastroenterol Hepatol, 2018, 2018: 4756147.
[3] LLOVET J M, de BAERE T, KULIK L, et al. Locoregional therapies in the era of molecular and immune treatments for hepatocellular carcinoma [J]. Nat Rev Gastroenterol Hepatol, 2021, 18 (5): 293-313.
[4] ZHU J, LOU Y, LIU P, et al. Tumor-related HSP70 released after cryo-thermal therapy targeted innate immune initiation in the antitumor immune response [J]. Int J Hyperthermia, 2020, 37(1): 843-853.
[5] BAUST J G, SNYDER K K, SANTUCCI K L, et al. Cryoablation: Physical and molecular basis with putative immunological consequences [J]. Int J Hyperthermia, 2019, 36(sup1): 10-16.
[6]李虎子,段振东,赵成,等.TACE联合冷冻消融治疗不可切除肝癌临床疗效的meta分析[J].介入放射学杂志,2021,30(8):804-813.
[7]刘川,雷丽程,朱丽,等.影像引导经皮冷冻消融术治疗肿瘤应用进展[J].中国介入影像与治疗学,2018,15(3):175-178.
[8] WU Q, LI J, YANG W. Survival analysis of patients with recurrent or metastatic soft tissue sarcoma who were treated by cryoablation: A real-world retrospective study [J]. J Cancer Res Ther, 2021, 17(7): 1736-1741.
[9] FILIPPIADIS D K, VELONAKIS G, KELEKIS A, et al. The role of percutaneous ablation in the management of colorectal cancer liver metastatic disease [J]. Diagnostics (Basel), 2021, 11(2): 308.
[10] GUPTA P, MARALAKUNTE M, KUMAR-M P, et al. Overall survival and local recurrence following RFA, MWA, and cryoablation of very early and early HCC: A systematic review and Bayesian network meta-analysis [J]. Eur Radiol, 2021, 31(7): 5400-5408.
[11] ZHANG W, GAO X, SUN J, et al. Percutaneous argon-helium cryoablation for small hepatocellular carcinoma located adjacent to a major organ or viscus: A retrospective study of 92 patients at a single center [J]. Med Sci Monit, 2021,27: e931473.
[12] YAKKALA C, CHIANG C L, KANDALAFT L, et al. Cryoablation and immunotherapy: An enthralling synergy to confront the tumors [J]. Front Immunol, 2019, 10: 2283.
[13] KIM D K, HAN K, WON J Y, et al. Percutaneous cryoablation in early stage hepatocellular carcinoma: Analysis of local tumor progression factors [J]. Diagn Interv Radiol, 2020, 26(2): 111-117.
[14]中国抗癌协会肿瘤介入学专业委员会,中国医师协会介入医师分会,中国临床肿瘤学会放射介入治疗专家委员会,等.冷热多模态消融治疗肝脏恶性肿瘤操作规范专家共识[J].中国介入影像与治疗学,2021,18(1):23-27.
[15] YANG Y, ZHANG Y, WU Y, et al. Efficacy and safety of percutaneous argon-helium cryoablation for hepatocellular carcinoma abutting the diaphragm [J]. J Vasc Interv Radiol, 2020, 31(3): 393-400. el.
[16] KIM R, KANG T W, CHA D I, et al. Percutaneous cryoablation for perivascular hepatocellular carcinoma: Therapeutic efficacy and vascular complications [J]. Eur Radiol, 2019, 29(2): 654-662.
